

Nurses utilize the Braden scale score as well as subscale scores to determine which nursing interventions to use, proving the importance of accurate scores (Tchato, Putnam, & Ruap; 2013). In one study, large variations were found amongst nurses’ interpretations of the Braden score, threatening the consistency and accuracy of Braden Scale. The Braden Scale, developed in 1987, consists of six sub-scales: 1. Sensory perception 2. Friction and shear The individual receives a score between 1-3 or 4 points for each sub-scale item. The sub-scales are then summed for. BRADEN PRESSURE ULCER RISK ASSESSMENT Home Health VNA Standard of Care: Braden Scale must be completed at Start of Care, Resumption of Care, Recertification, and change in patient condition. SENSORY PERCEPTION: Ability to respond meaningfully to pressure-related discomfort. Per Braden Scale Sub-scale Score. If Sub-scale score is 1 or 2: Intervention Sensory Perception Pay extra attention, looking for subtle signs of pressure damage, as the patient is not able to report pain Moisture Check frequently if incontinent. Keep skin clean and dry. Use Calazime on perineal area and buttocks. Change linens as needed to keep. The above Braden scale for predicting Pressure Sore risk chart provides the chart with different score according to the category. On adding the scores in the Braden scale Pressure Ulcer table, the overall score can fall between 6 to 23 and the lower score indicates the higher risk.
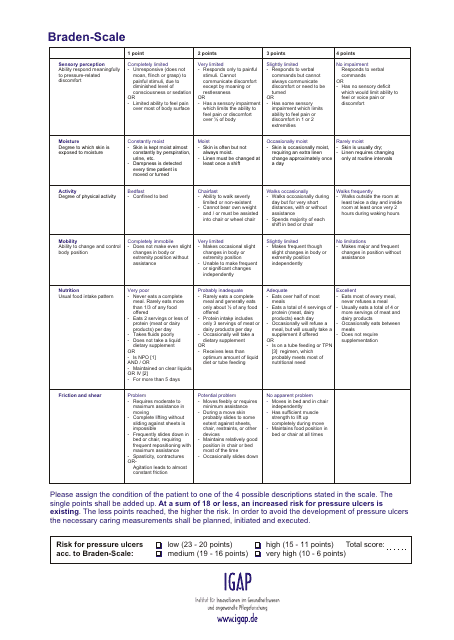
Printable Braden Scale Assessment Form
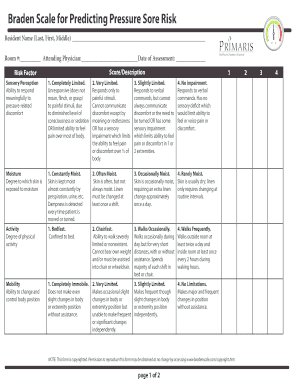
Printable Braden Scale Assessment
Poor nutrition, intravascular volume depletion, and peripheral vascular disease can each lead to unhealthy skin and impaired wound healing, which in turn increases the risk of developing pressure ulcers. Low body weight is also a concern. Weight less than 119 pounds or a body mass index (BMI) less than 20 indicates increased risk for pressure ulcer development [80].
Recent weight loss, decreased nutritional intake, inadequate dietary protein, and impaired ability to feed oneself have been identified as risk factors for pressure ulcer development. An estimated 50% of elderly patients admitted to hospitals have suboptimal protein nutrition [80]. When there is a sustained deficit of protein as an energy source, skin and soft tissues become more vulnerable to injury. In managing patients with pressure ulcer, or those at risk, the amount of protein in the diet appears to influence prognosis for recovery and prevention. In one study, patients who received a 24% increase in protein intake had significant improvements in ulcer healing and prevention of new skin injury compared to those who received a 14% increase [24].
Poor nutrition, intravascular volume depletion, and peripheral vascular disease can each lead to unhealthy skin and impaired wound healing, which in turn increases the risk of developing pressure ulcers. Low body weight is also a concern. Weight less than 119 pounds or a body mass index (BMI) less than 20 indicates increased risk for pressure ulcer development [80].
Printable Braden Scale Blank Form
Recent weight loss, decreased nutritional intake, inadequate dietary protein, and impaired ability to feed oneself have been identified as risk factors for pressure ulcer development. An estimated 50% of elderly patients admitted to hospitals have suboptimal protein nutrition [80]. When there is a sustained deficit of protein as an energy source, skin and soft tissues become more vulnerable to injury. In managing patients with pressure ulcer, or those at risk, the amount of protein in the diet appears to influence prognosis for recovery and prevention. In one study, patients who received a 24% increase in protein intake had significant improvements in ulcer healing and prevention of new skin injury compared to those who received a 14% increase [24].